Every clinician has a unique style of making their notes! With Empathia AI, it has never been easier to cater to your specific style! Empathia AI offers many changes to note styles, including adjustments in content length and formatting, narrative vs point-form, keeping it simple or detailed, and more! Users can also toggle with problem-based History of Present Illness (HPI), Assessment and Plan sections. This article dives deep into each specific setting of Note Style.
Benefits of Changing Note Style:
Consistency: Standardized styles ensure uniform quality across notes.
Flexibility: Providers can switch between styles based on their needs.
Efficiency: Simplified formats save time, allowing more focus on patient care.
Faster Documentation: Shorter entries reduce paperwork time.
Better Organization: Improved structure makes it easier to find important information. Detailed notes in narrative or point form are more organized when they become complex.
Tailored HPI: Problem-based histories allow for more relevant and accurate documentation.
Below are descriptions of some of the feature we have on "Note Style":
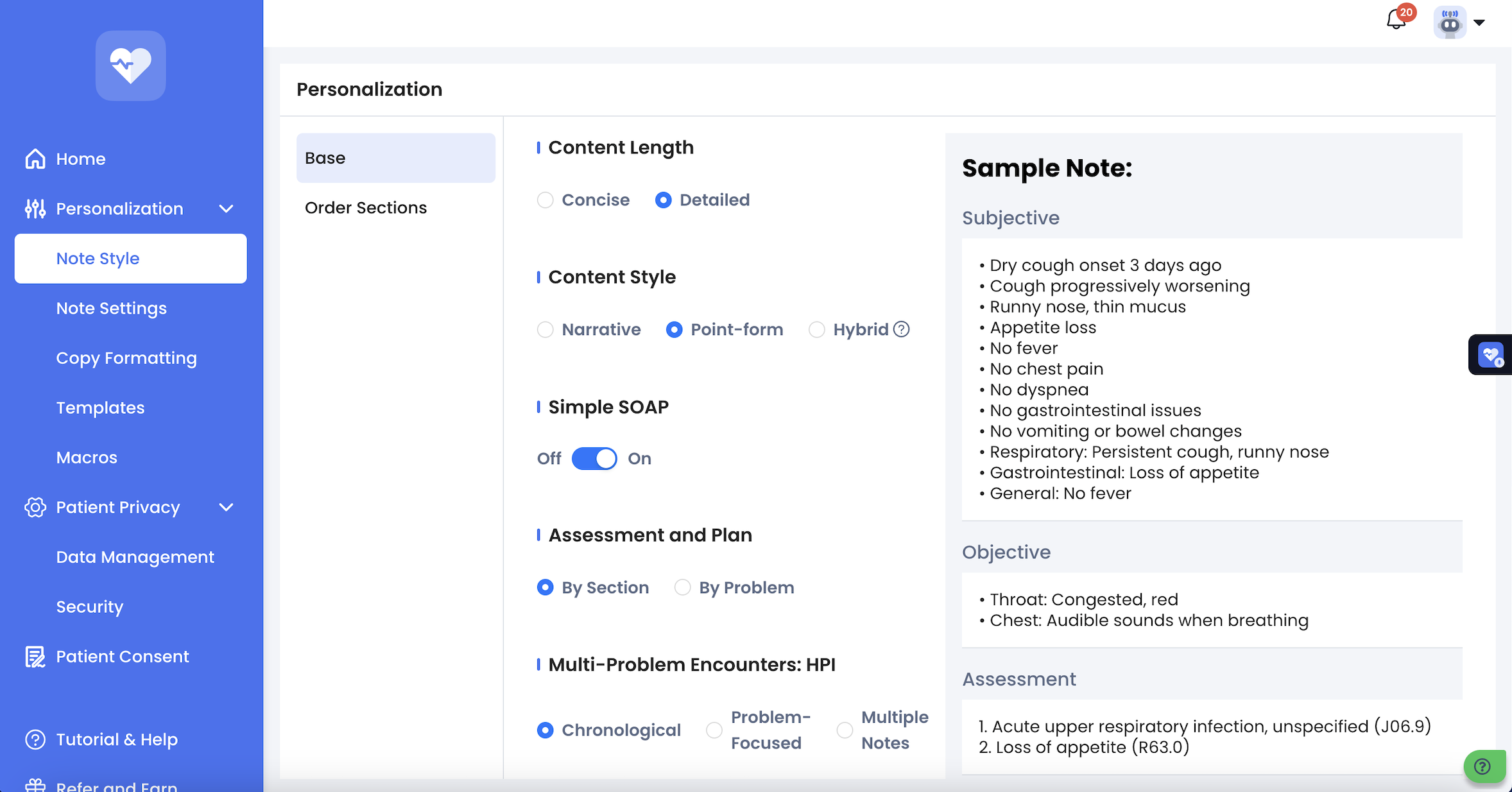
1) After clicking "Note Style" which is located on the left side panel, you will see the screen shown below.
A note that is concise will be:
Shorter
To the point
Focus on main ideas
Have less detail
Easier to review quickly
A note that is detailed will be:
More thorough
Descriptive
Include specific information and examples
Be better for in-depth understanding
Can be more time-consuming to review
Below is a visual representation of this.

A note that is in narrative form will have sentences like this --> "The patient had pneumonia three years ago".
A note that is in point form will have sentences like this --> "-Pneumonia 3 years ago".
A note that is in hybrid form will have certain subsections in narrative form and certain subsections in point form. You can select which subsections you would like to have in narrative format. Below is a visual representation of this.

A simple SOAP note will have certain sections combined and be put into one. For example, HPI, past medical history, family history, social history will all be put into separate sections when "Simple SOAP" is off. They will be put into one "Subjective" when "Simple SOAP" is on. Below is a visual representation of this.


The "HPI" and "Assessment and Plan" can be organized based on problems. Please refer to the article titled "Organize Notes - HPI and Assessment and Plan By Problem" for more details on this feature. Below is a visual representation of this.

When "Patient Consent" is on, the following sentence will appear at the end of each note --> "Informed consent was obtained from this patient for Empathia AI-assisted ambient charting. Accuracy of the note has been verified by your clinician". Below is a visual representation of this.

Lastly, you can "Hide Subsections" of your note. For example, you can hide sections such as social history, review of systems and they won't appear in any of your notes. You may also choose to hide or show the sections which are empty and don't have any information in them. Below is a visual representation of this.


If you have any questions, please contact support@empathia.ai
We are always here to help!
Was this article helpful?
That’s Great!
Thank you for your feedback
Sorry! We couldn't be helpful
Thank you for your feedback
Feedback sent
We appreciate your effort and will try to fix the article